Allergy Office: Integrating NPs/PAs
Introduction
You’ve most likely heard how helpful nurse practitioners (NPs) and physician assistants (PAs) can be to allergy practices – and you may even employ an NP or PA. But how much do you really know about them? Try your hand at this little quiz to find out!
How did you do? Did anything surprise you?
In this module, you’ll learn all about NPs and PAs and the great service and value they can add to allergy practices. You’ll explore...

- What NPs and PAs are
- How they can help allergy practices
- State and federal regulations, as well as licensing requirements
- Their scope of practice and prescriptive authority
- How to get reimbursed for their work
- Whether you need to add a physician or an NP or PA to your practice
- How to successfully integrate an NP or PA into your practice
The possibilities that NPs and PAs can offer your practice are exciting, so let’s get started!
What Exactly Are NPs and PAs?
NPs and PAs are both advanced practice clinicians, or APCs, so that’s how we’ll refer to them throughout this module. (Note: they generally don’t like being called mid-levels or physician extenders, which can wrongly imply a lower level of care. So please avoid those terms out of professional respect.) APCs are qualified health care professionals who have undergone specialized education, training, certification and licensure enabling them to provide care and treatment to patients. They have been certified to perform some of the same tasks as a physician, and they frequently work under the close supervision of a physician. Studies have shown comparable quality of care for NPs and PAs relative to physicians.1 Their scope of practice, level of independence and authority vary by role and by state.
APCs’ scope of practice, level of independence and authority vary by role and by state.
So, what are some of the things they can do? APCs can...

- Evaluate patients
- Perform examinations
- Make diagnoses
- Educate patients
- Prescribe medications
- Order and interpret diagnostic testing
In essence, APCs can function autonomously with physician oversight – according to practice agreements and state requirements.
NPs and PAs go through considerable training before being licensed and certified. They have advanced degrees and must complete practical clinical training. Here’s a breakdown of what it takes to become an NP or a PA:
| Nurse Practitioner | Physician Assistant |
|---|---|
| State Board of Nursing licensure (RN, APRN) | State-specific licensure to practice |
Nationally board certified by AANP or ANCC
| Nationally board certified by NCCPA
|
Renew certification every 5 years by:
| Complete a recertification exam every 10 years AND Complete 100 hours of CME every 2 years. |
| (*APRN – Advanced Practice Registered Nurse; AANP – American Association of Nurse Practitioners; ANCC –American Nurses Credentialing Center; NP-C – Nurse Practitioner, Certified; APRN-BC – Advanced Practice Registered Nurse, Board Certified; NCCPA – National Commission on Certification of Physician Assistants; PA-C – Physician Assistant, Certified) | |
As you can see, APCs are thoroughly trained and highly skilled. Plus they bring a vital, valuable collaborative approach to medical care. Let’s see specifically how this works in an allergy practice next.
How APCs Can Help an Allergy Practice
APCs can bring substantial benefits to your practice. When done effectively, employing APCs can...
- Increase practice revenue at a lower cost. APCs can provide many of the same services as allergists but cost practices less in overhead than a physician.
- Enhance the quality of care for patients through better access and coverage.
- Improve physician satisfaction and reduce burnout by sharing the workload.
Just like a physician, APCs can have their own schedule of patients. However – and this is an important difference – APCs need to discuss all complicated patients with the physician. So you’ll need to set criteria for determining when this is necessary.
What types of services do NPs and PAs provide in allergy practices? The College’s Practice Management Committee shared the following list of services APCs provide in their practices:
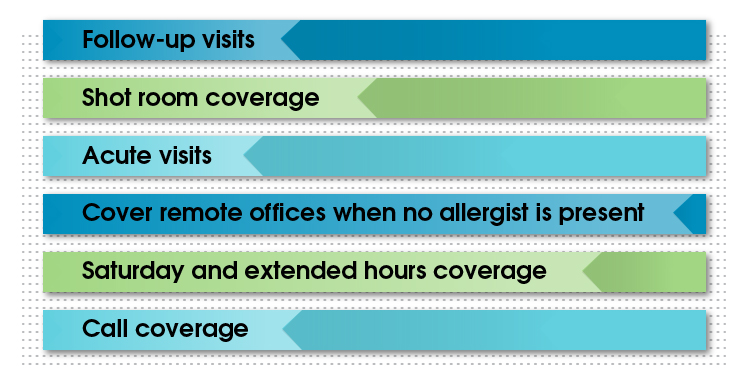
Just a note about acute visits – these include urgent, day-of appointments and short-notice testing. You may want to consider blocking slots in an APC’s schedule for same-day appointments so you can ensure patient access for urgent visits. This is especially handy during busier times like peak pollen season.
Whatever you do, don’t make the mistake of using an APC to do things an RN can do. Make sure APCs are working at the top of their license, which means working on the most complex and challenging tasks their licenses, training and abilities allow. It simply isn’t cost-effective to have APCs spend time on tasks that could be done by someone with less training.
Things to Consider When Adding an APC
Are you intrigued by the idea of adding an APC to your practice? Then let’s look at two important practical considerations before bringing one on board:
- Licensing requirements (both state and federal), scope of practice and prescriptive authority
- How you’ll bill for your APC’s services
Let’s break these down in some detail.
Licensing Requirements, Scope of Practice and Prescriptive Authority
Start by researching the licensing requirements and scope of practice for APCs in your state.
To determine the state and federal licensing requirements for NPs and PAs, refer to the following organizations and/or your state medical society:
| NPs | PAs |
|---|---|
| American Association of Nurse Practitioners (AANP) | American Academy of Physician Assistants (AAPA) |
The scope of practice for APCs, as well as their prescriptive authority, is regulated at the state level, so it can vary widely. Also, agreements regarding supervision and how APCs will collaborate with physicians are governed by each state. Supervision requirements have changed over the past several years, with more states providing expanded practice options for NPs. As of July, 2024, NPs are allowed to practice without an agreement with a specific physician in 27 states and the District of Columbia.
To make matters more complicated, in some states, federal regulations may be more restrictive than state regulations. So you really need to know the laws for your particular state as well as federal regulations.
Finally, local Medicare Administrative Contractors (MACs) may also have separate restrictions on services provided by APCs. For example, one MAC currently doesn’t allow allergy testing by APCs. So be sure to check your local MAC requirements as well.
Reimbursement
The next area to research when considering adding an APC to your practice is reimbursement. There are two ways you can bill for the services provided by APCs. Let’s start with how Medicare handles billing, since private payers usually follow their lead.
Medicare

With Medicare, you can bill one of two ways:
- Bill directly under the NP or PA, using their own National Provider Identifier (NPI). There will be a 15% reduction in reimbursement with this method. (The reduction is about the same for commercial payers.)
- Bill "incident to," which means billing under the supervising allergist's NPI. With this option, you'll be reimbursed at 100% of Medicare rates.
Who wouldn’t prefer 100% reimbursement? However, you need to meet certain requirements to bill "incident to":
- The allergist must initiate the patient’s care and any changes in the care plan.
- The allergist must be present in the office suite and available during the time the care is given.
- An allergist must actively participate in and manage the patient’s course of treatment.
So APCs can’t see new patients, or existing patients with new problems, and bill as "incident to." Also, if an allergist isn’t in the office at the time of visit, you can’t bill "incident to." There’s a little twist with this second point: though a physician does have to be available at the time of care and must manage the care, the supervising physician can be any doctor in the group – he or she doesn’t have to be the one who initiated and manages the patient’s care.
Private Payers
Many commercial payers follow Medicare’s "incident to" rules, but more are starting to require billing directly under the NP or PA. But plans may vary, so be sure to check your contracts with commercial payers and review their rules for "incident to" billing. Also, some commercial plans have less restrictive rules regarding "incident to" billing – but make sure you have this in writing!
Which Billing Method Is Right for You?

Figuring out which way to bill for an APC’s services depends on how APCs will work in your practice, in addition to state regulations and insurance company or MAC requirements. For instance:
- Will your APC see only follow-up patients and cover allergy shots, and will there always be an allergist in the clinic with them? If so, "incident to" billing might work.
- Or will your APC need to see new patients, cover remote locations by themselves, or cover extended hours and Saturdays by themselves? In that case, billing "incident to" won’t work.
- If you’ll have multiple APCs working at your practice, will they all provide the same services? Or will some be more independent than others?
Some practices take a mix-and-match approach, using "incident to" billing for some APCs and billing under APCs’ NPIs for others. This can get complicated, however, and you need to make sure you’re scheduling only appropriate patients for APCs billing "incident to" (no new patients or patients with new problems, for example).
Whichever method(s) you choose, make sure they meet the insurer’s criteria (whether Medicare or a private payer), state regulations, and try to maximize revenue for the practice.
Note: it is generally beneficial to credential APCs with all plans that allow it - even if you are planning to bill “incident to”. This way, if the APC must bill under their own NPI number for any reason (either practice circumstances change or the insurer requires it), then claims won't hit a snag. (Remember, credentialling can be a 3-to-4-month process, so advanced planning is a must.) Another tip: consider adding a longer two-sided notice of termination provision to the APC’s contract to avoid being left with a difficult coverage situation and little notice.
When to Consider Adding APCs to Your Practice
Okay, so you’re excited about everything an APC can add to your practice. When is the right time to add one? One or more of the following could indicate a need for an APC:
- When the demand for your services begins to exceed your practice’s capacity or you’re considering expanding.
- If you need help with call coverage, coverage for vacations or absences, and supervising immunotherapy.
- If one or more allergists are planning to retire or leave and you need a replacement.
There’s no easy formula for when it makes sense to add a new allergist, but you’ll want to consider the following statistics together over time:
Third Next Available appointment for each allergist
This is a snapshot in time that says, if Patient X requests an appointment with Allergist Y today, how many days would they have to wait for the third next available appointment? This measure indicates how easy it is to schedule appointments with your allergists. (We don’t use first and second available appointments because they may be available due to last-minute cancellations). If the Third Next Available appointment is far out, you aren’t meeting patient demand and may need to add a allergist.Physician and APC fill percentages
This refers to the percentage of available appointments that are filled each day, not counting no-shows. Are you consistently at higher than 90%? If so, you may need to add a allergist.
So, what is the right “target” number for Third Next Available appointment? It depends to a degree on your market and competition. Some allergy practices may be fine with a Third Next Available new patient appointment of 30 days – if your competition takes 60 or more days to see new patients. But generally, patients prefer to see someone sooner, so two to three weeks may be more appropriate.
Add a Physician or an APC?
If you do determine that it’s the right time for your practice to add a allergist, how do you decide whether to add a physician or an APC?
The right answer for your practice depends on many things:
Bottom line: Consider your practice needs and how you would use the new allergist.
Bringing an APC on Board
Once you decide you do want to bring an NP or PA on board, you’ll want to do two things to make the new addition a success: Look for certain qualities when hiring, and integrate them effectively into your practice.
Qualities to Look For
Finding the right fit is essential when adding an APC to your practice. You’ll want to find an NP or PA that has...
- A team-based approach
- A collaborative spirit
- Adaptability to the physician’s style of medicine (as well as sharing the physician’s philosophy on medicine)
- A patient-centered work ethic
- Excellent communication skills (able to explain things to patients plus communicate well with physicians)
- A willingness to see patients independently - if your practice requires this.
As with any staff member, you want someone who fits in with the culture of your practice.
Note: both the American Association of Nurse Practitioners2 and the American Academy of Physician Assistants3 post jobs on their websites, so they are good resources for practices looking to hire APCs.
Successfully Integrating a New APC
How do you successfully integrate a new APC into your practice? Here are a few tried-and-true ideas:
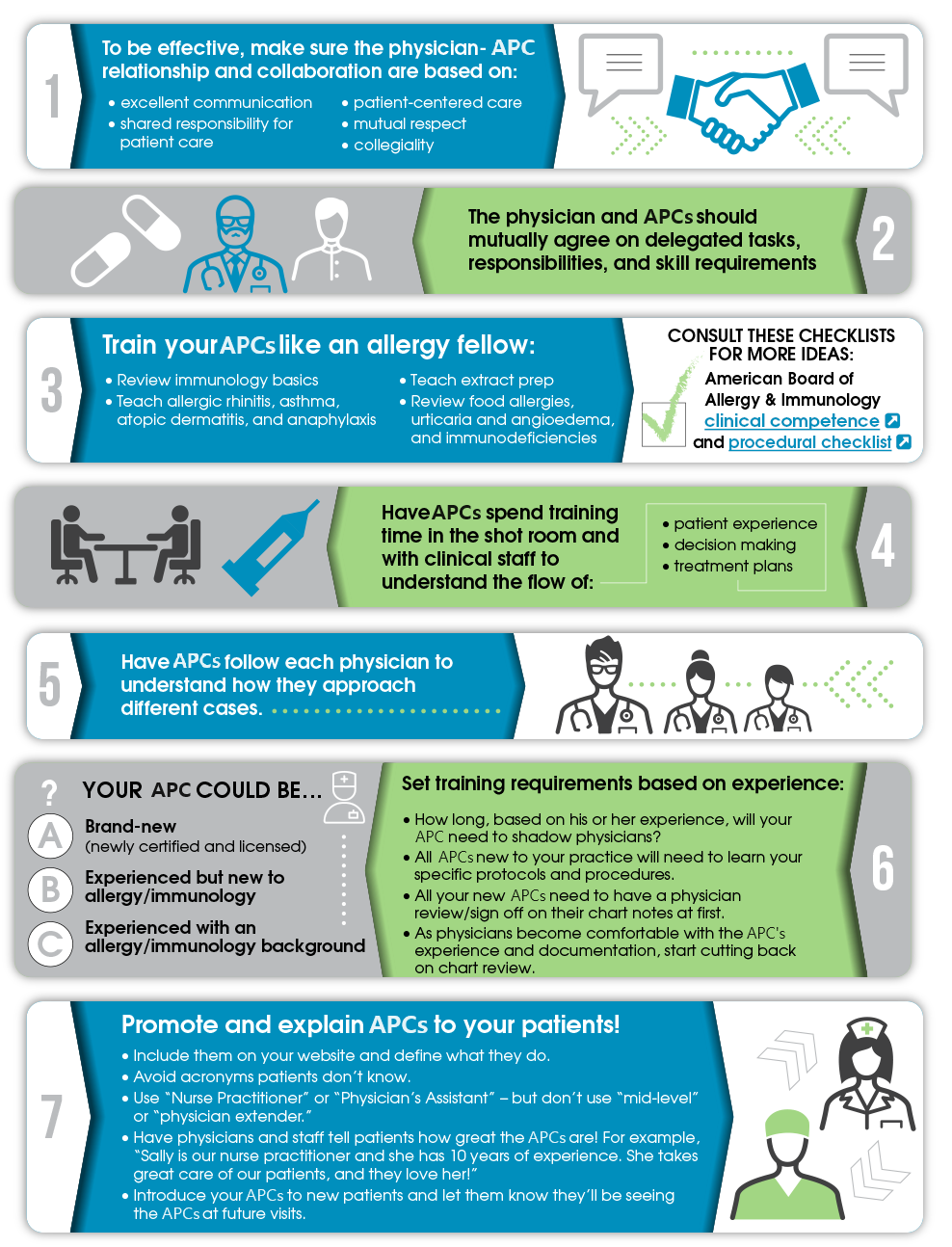 Clinical competence Procedural checklist*Consider requiring all new APCs to manage 10-20 shot reactions before they are left alone in an office. During this time, all charts should be reviewed with their supervising physician.
Clinical competence Procedural checklist*Consider requiring all new APCs to manage 10-20 shot reactions before they are left alone in an office. During this time, all charts should be reviewed with their supervising physician.
If you follow these tips, you’re bound to successfully integrate your APC in no time!
Finally, encourage your new NP or PA to become a College member, where they can find a wealth of educational resources for allergy and immunology allergists and opportunities to network with and learn from other APCs in our specialty.
Conclusion
Since we started with a quiz, let’s conclude with one also. This will help reinforce what you’ve learned in this module.
Hopefully, your answers revealed that you’re up on your APCs!
If you think your practice could benefit from bringing an APC on board, take some time to plan out your next steps:
- What’s the scope of practice allowed in your state?
- What are the regulations in your state, and how do they compare to federal regulations?
- How will you use APCs in your practice? In other words, what specific needs does your practice have that you want them to meet?
- How will you bill for your NP or PA?
- How can you best integrate them into your practice?
Choosing to make an NP or PA part of your team can greatly improve patient access and the quality of your patient care. Just make sure to do your research thoroughly – especially when it comes to state and federal licensing and regulations. The right APC, under the right circumstances, will only enhance your practice!
Resources
- American Academy of Physician Assistants (AAPA), Physician Assistant State Licensing Requirements (See state-by-state licensure laws for physician assistants.)
- American Academy of Physician Assistants (AAPA), Employer Resources for Hiring Physician Assistants. The AAPA has combined a series of employer tools for physician assistants.
- American Association of Nurse Practitioners (AANP), Nurse Practitioner State Practice and Licensure Laws (See state-by-state licensure laws for nurse practitioners.)
- ACAAI, "Are you billing correctly for nurse practitioners and physician assistants?"
- Jeff Morris, MD, MBA, FACS, FRCS(C), Optimizing the Value of Advanced Practice Clinicians
- National Council of State Boards of Nursing
- MGMA: Medical groups turn to advanced practice provider roles amid staffing struggles

 Facebook
Facebook X
X LinkedIn
LinkedIn Forward
Forward