Coding for Immunotherapy
Introduction
Immunotherapy can make your patients’ lives so much easier – but coding for it is no picnic, right?
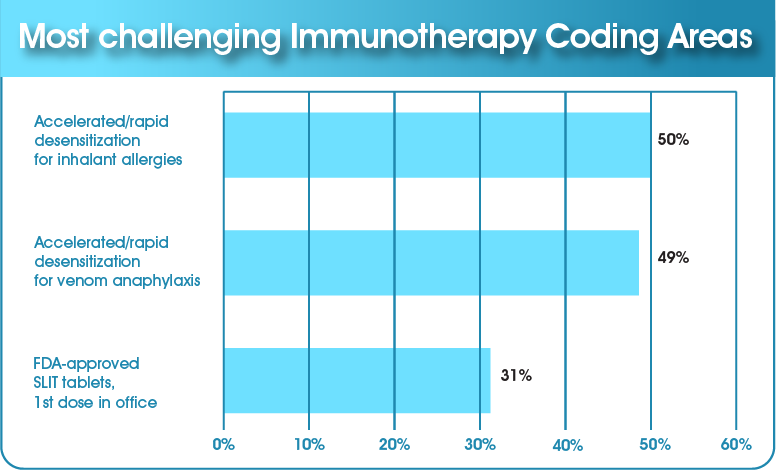
In a recent College webinar, we took a poll of allergists and their staff, asking what their challenges with coding for immunotherapy are. Do their frustrations match your experience?
Let’s see if we can make coding for immunotherapy treatment less complicated and more clear. In this module, we’ll explore these types of immunotherapy and the coding guidelines for them:
- Inhalant allergen immunotherapy, including
- Sublingual immunotherapy (SLIT)
- Subcutaneous immunotherapy (SCIT)
- Venom immunotherapy
Coding for immunotherapy may never be a walk in the park, but it certainly doesn’t have to be a treacherous journey! So jump into your sneakers, grab a bottle of water and let’s get started!
Inhalant Allergen Immunotherapy

Immunotherapy for inhaled allergens (aeroallergens) includes two methods: sublingual and subcutaneous. Let’s investigate each of these.
Sublingual Immunotherapy (SLIT)
For patients who don’t do well with needles, under-the-tongue immunotherapy is a nice alternative. One method of SLIT is FDA-approved: tablets; while the other isn’t yet: liquid extract drops. Of course, FDA approval will impact whether insurance may pay for the therapy or not.
FDA-Approved SLIT Tablets
Currently, the FDA has approved SLIT tablets for three allergens:
 Grass
Grass Ragweed
Ragweed Dust mites
Dust mitesThe coding for SLIT tablets is a little tricky. Why? Because there’s no CPT code for SLIT – even for the first dose administered in the office. So what are your options?
Well, you may lean toward CPT 95076, for an ingestion challenge, but this won’t work. This code is for a diagnostic test that requires sequential and incremental ingestion of the food or drug. And that’s not what’s happening with SLIT.
SLIT ≠ Ingestion
A possible alternative is to use an E/M code – if the doctor administers the first dose during an education/counseling session. For this to be appropriate, the physician could explain how to take the tablet, what the possible reactions could be (including anaphylaxis), how to use an epinephrine auto-injector, and so forth. The physician must spend this time with the patient and should document all these items of medical care in the chart.
E/M code means MORE than just giving the dose!
Finally, sublingual immunotherapy tablets are not FDA-approved for anyone over the age of 65. As a result, Medicare doesn’t cover sublingual immunotherapy.
Liquid Extract Drops
This form of treatment is not FDA-approved, so insurance may not pay for it at all. In fact, some carriers consider this to be experimental.
As you’d expect, there’s no CPT code for this.
- Don’t try to use CPT 95165. This applies only to subcutaneous immunotherapy, so it’s not appropriate.
- Avoid using CPT 95199 for "unlisted allergy services." This isn’t a reliable code – it’s frequently rejected and rarely paid (not a winning combination).
So what should you do? We recommend you check with the insurance company first to see if they reimburse for this service. Do this before providing the treatment to the patient! Currently, the majority of third-party payers don’t pay for SLIT drops. It’s OK to charge the patient cash if they’re willing and able to pay for the therapy.
Coding for subcutaneous immunotherapy is much clearer.
Subcutaneous Immunotherapy (SCIT)
For managers/billers unfamiliar with different types of SCIT, let’s do a quick review of the three methods we’ll be discussing. Keep in mind the times shown are only examples and can vary.
| Conventional (Buildup Schedule) | Cluster (Accelerated) | Rush (Rapid Desensitization) |
|---|---|---|
| 1-3 times per week 30-minute observation in office after injections | 2 times per week 1-3 hour appointment each time | 1 or 2 days total Up to several hours per appointment |
| Single dose of antigen(s) each visit | 2 or more doses per visit | Multiple doses |
| 3-6 months to reach maintenance | 4-8 weeks to reach maintenance | 1-2 days to reach maintenance |
Now let’s take a look at the coding for each of these.
Conventional SCIT Coding
95115
This code is for "professional services for allergen immunotherapy not including provision of allergenic extracts; single injection."
95117
This code is for "2 or more injections."
95165
“Professional services for the supervision of preparation and provision of antigens for allergen immunotherapy; single or multiple antigens (specify number of doses).”
To sum these up, you’ll bill either 95115 or 95117 for the administration of the injection. You cannot bill both on the same day.

For 95165, you’ll bill the number of anticipated doses per your buildup schedule. Billing for 95165 can be complicated, and it differs for Medicare and commercial payers. We won’t review it here, so for more information, check out our webinar Everything You Wanted to Know about CPT 95165 or our 15-minute educational module Allergy Office: Coding 95165.
Cluster (Accelerated) and Rush (Rapid Desensitization) SCIT
There isn’t a specific CPT code for cluster or rush immunotherapy – but there is a time-based code for rapid desensitization: 95180. Since both cluster and rush immunotherapy are forms of rapid desensitization, this is the code we recommend for both.
Here’s how 95180 works:
- It’s based on time – you’re paid by the hour.
- Time means the total time spent to administer doses and to closely and carefully monitor the patient throughout the desensitization process. This includes taking vital signs, doing careful observation between each injection, etc. There’s significant physician work and significant risk (anaphylaxis) with this type of SCIT.
- The billing formula for 95180 looks like this:
- 95180: Rapid desensitization procedure, each hour (e.g., insulin, penicillin, equine serum)
- Charge by time: # _____ hours = # ______ units
- Time equals total time spent to administer doses and to closely and carefully monitor the patient throughout the desensitization procedure.
- A minimum of 31 minutes (just over half the time) is required to bill the first hour, and a minimum total of 91 minutes is required to bill a second hour.
- Since you’re billing by the number of hours, documentation is especially key! Use a flowchart to support the time it takes for desensitization. Also, be sure to document the medical necessity for the procedure.
Document, document, document!
- Note: 95180 includes administration, so don’t bill with 95115 or 95117.
- It’s likely that extract preparation (95165) has already been billed. If this is the case, don’t bill for it again.
When it comes to coding and billing for rapid desensitization, it’s wise to check with your payers for their coverage guidelines regarding diagnoses. Some insurance may cover 95180 for certain diagnoses (venom, drug, inhalant allergies, etc.) but not others. As you know, ICD-10 and CPT codes must be paired, so make sure the diagnosis you’re using is appropriate for 95180.
In general, Medicare and Medicaid pay for both cluster and rush therapy. However, local carriers may have different coverage than the national carrier. So always check with your local carrier to find out what their particular policy is.
How are you doing with all of this? Perhaps a couple of examples would help cement everything in your mind.
Cluster Immunotherapy Example
Jamal comes in for his cluster (accelerated) immunotherapy treatment. You give him multiple injections every 30 minutes at each visit, using multiple vial sets (for pollens and molds).
Jamal receives multiple injections from each vial set for 96 minutes. He is carefully monitored the entire time.
How should you bill for this? Remember the formula: _____ # of hours = _____ # of units. Since the treatment was an hour and 36 minutes, you’d bill for 2 hours (36 minutes is more than half of one hour, so it counts as the whole hour). So here’s how you should charge:
2 hours = 2 units of 95180
Remember, multiple injections don’t affect how you bill: 95180 is a time-based code!
Rush Immunotherapy Example
Lorna arrives for her rush (rapid desensitization) immunotherapy treatment. You give her multiple injections every 30 to 60 minutes, using multiple vial sets (pollens, molds and dust mites). She’s carefully monitored the entire time.
Lorna gets 8-10 injections over 6 hours’ time. So here’s how you’d bill:
6 hours = 6 units of 95180
So that’s how you code for inhalant allergen immunotherapy. Next, let’s tiptoe carefully into the venturesome world of venoms.
Venom Immunotherapy
When it comes to venom immunotherapy, keep in mind you have separate codes for the extracts and the injections. Let’s look at extracts first.
Venom Extract Codes
Coding for venom immunotherapy extract is different from coding for aeroallergen immunotherapy extract. With aeroallergen therapy, when the treatment kit is prepared, you might not bill for it again for another year, when the maintenance vial expires. But with venom immunotherapy, you typically bill the venom extract codes with each injection visit, along with the injection code.
Also, you won’t use code 95165 (the aeroallergen extract code) at all. Instead, five different codes cover the cost of the venom and the preparation of the dilution sets:
| Code | Definition |
|---|---|
| 95145 | 1 insect |
| 95146 | 2 insects |
| 95147 | 3 insects |
| 95148 | 4 insects |
| 95149 | 5 insects |
What might these extracts be? There are six types:
| Types of Venom Extracts |
|---|
Honeybee  |
Wasp  |
Yellow jacket  |
Yellow hornet  |
White-faced hornet  |
| Mixed vespid: • Yellow jacket • Yellow hornet • White-faced hornet  |
So that’s the scoop on extracts. Next, let’s hover over to injections.
Venom Injection Codes
Ah, we’re in luck! The injection codes for venom immunotherapy are the same as those for aeroallergen immunotherapy:
| 95115 | 1 injection |
|---|---|
| 95117 | 2 or more injections administered at the same time |
| 95180 | Cluster or rush injection administered in a series of 1 or more injections, typically 30 minutes apart |
Take a look at the following examples to get a better grip on how this coding works.
Conventional Venom Immunotherapy: Example 1
Peter, who’s allergic to honeybees and wasps, shows up for his first injection. Every visit would be the same both during the buildup and when on maintenance. Here’s how you’d code the claim:
- 95117: 2 or more injections, one with honeybee venom and one with wasp venom
- 95146: 2 insects (honeybee and wasp)
Conventional Venom Immunotherapy: Example 2
Your mixed vespid allergic patient, Christine, shows up for her first injection. As in the previous example, every visit would be the same both during the buildup and when on maintenance. So here’s how you’d code the claim:
- 95115: 1 injection with mixed vespid venom
- 95147: 3 insects (remember, mixed vespid contains 3 insects: yellow jacket, yellow hornet and white-faced hornet)
Cluster and Rush Venom Immunotherapy: Example 1
(This is a little trickier – especially for the venom extract coding.) Gabriela, who is allergic to honeybees, comes in for her first treatment. She can stay for an hour, so she’ll get a cluster set of injections every 30 minutes. (Every cluster visit would be the same.) Here’s our cluster schedule (2 injections administered during this visit):
- 08:00 - 0.1 mL of 1 mcg of honeybee venom administered
- 08:30 - 0.2 mL of 1 mcg of honeybee venom administered
So here’s how you’d bill the claim:
- 95180: 1 unit = 1 hour, which is how long Gabriela will be in the clinic
- 95145 (2 units): 1 insect (honeybee) but 2 doses given
Cluster and Rush Venom Immunotherapy: Example 2
Your honeybee and mixed vespid allergic patient, Juan, shows up for his first treatment and can stay for an hour. So he’ll get a cluster set of injections separated by 30 minutes (with every cluster visit being the same). Here’s how you’d code the claim:
- 95180: 1 unit = 1 hour, which is how long Juan will be in the clinic
- 95148 (2 units): 4 insects, honeybee and mixed vespid (which has 3 insects: yellow jacket, yellow hornet and white-faced hornet); however, 2 doses of the 4 insects is given
Remember: you administered 4 injections during this visit, but the number of injections doesn’t matter! For cluster immunotherapy, you use 95180, which is based on time rather than the number of injections administered.
Cluster and Rush Venom Immunotherapy: Example 3
Schuyler, your honeybee allergic patient, is right on time for his first injection. He’ll be in the clinic all day (8 hours) for a rush schedule with 8 injections given every 30-60 minutes. So here’s how you’ll bill this:
- 95180: 8 units (1 unit = 1 hour, so 8 units = 8 hours)
- 95145: 8 units – 1 insect (honeybee) but 8 separate doses given throughout the day
Be sure you document medical necessity. Also, the time for 95180 is while Schuyler is being intensely monitored – not when he signs in and leaves.
Can You Code Like an Expert?
Do you feel like you’re getting the hang of this? After all, we don’t want you getting “stung” by using the wrong codes! (Is there immunotherapy for bad puns?)
To test your coding expertise, try your hand at the following quiz.
Does it seem like immunotherapy coding will be a picnic now? Or are there still some troublesome ants and the threat of rain to make that picnic less than perfect? Don’t worry, if you need more help with the pesky aspects of coding for immunotherapy, we have just the resources for you. Check them out below, and let us know how you’re doing!
College Coding Resources
- Immunotherapy Coding Essentials Our coding experts, M. Razi Rafeeq, MD, FACAAI, and Mike Tankersley, MD, MBA, FACAAI, do a deep dive into the coding for various types of immunotherapy in this webinar. (July 18, 2019)
- College Coding Toolkit

 Facebook
Facebook X
X LinkedIn
LinkedIn Forward
Forward