Module 1: Biologics Billing Basics
Introduction
Have you ever had a nightmare where you’re trying to cross a busy street, but something is making you move in slow motion? You’re partway through the crosswalk, and the light is changing, but for some reason you can’t get your legs to move any faster. It’s frustrating and scary at the same time!
Well, for many practices, handling the billing and management of biologics feels pretty similar. You know what your patients need and you’re trying to get it to them, but the prior authorization process and just managing biologics in your practice saps so much of your resources you fear you won’t be able to deliver the care to your patients.
In this module, we’ll discuss some options to provide the much-needed relief biologics offer for patients without breaking your practice. We’ll look at...

- Tips and tricks for dealing with prior authorizations
- Options for providing this beneficial medication
- Things to consider if you opt for a buy-and-bill approach
- Helpful details regarding reimbursement and coding
- How to decide which approach(es) will work best for your practice
The benefits of biologics can be a dream come true for your patients, so let’s help your practice get moving and providing patients what they need!
The Prior Authorization Challenges of Biologics
It probably won’t surprise you to learn that some practices "spend an average of two business days a week per physician" just doing prior authorizations (PAs). 1
That’s astounding!
All that time could go to patient care, but instead it’s getting sucked into the quicksand of frustrating paperwork and phone calls with insurers.
Some practices spend an average of 2 business days per week per physician just doing PAs.
Unfortunately, when it comes to biologics, you’ll be facing the prior authorization gauntlet with most insurance companies.
On the plus side, however, ACAAI has created a Prior Authorization Toolkit that can help you streamline this process. Here you’ll find detailed tips and tricks for making the process easier, such as:
- Creating policies and procedures to stay organized. Remember, it’s easier to stay ready than to get ready!
- Taking advantage of technology. Rather than fill in paperwork by hand, make phone calls or (gasp!) send faxes, send your information electronically.
- Getting your patients involved in the process. Patients can call their insurance companies or ask their company’s benefits manager to intervene on their behalf. Finally – and this can be a game changer – some drug manufacturers have programs to help patients afford expensive biologics. The more help with PAs, the better!
The College’s Prior Authorization Toolkit also has a groundbreaking PA appeal-letter generator for specific biologic/disease combinations – and we’ll be adding new biologic letters as new drugs become available:
| Condition | Medication |
|---|---|
| Allergic Rhinitis | Odactra |
| Anaphylaxis | Neffy |
| Asthma | Cinqair, Dupixent, Fasenra, Nucala, SMART, Tezspire, Xolair |
| Atopic Dermatitis | Dupixent |
| Chronic Urticaria | Xolair |
| Food Allergy | Xolair |
| Nasal Polyps | Dupixent, Xhance |
| Peanut Allergy | Palforzia |
These appeal letters are scientifically based, complete with literature references, and are customized to each patient. You can download them in Microsoft Word and edit each one as necessary. College membeOdactrars have had great success with these letters, so give this tool a try the next time a PA is denied.
Finally, the Prior Authorization Toolkit includes valuable patient education resources, including articles on how to save money on prescription drugs as well as short videos that explain step therapy, PAs and more. An educated patient is an empowered patient!
Next, let’s explore your options for providing biologics to your patients.
You Have Options!
Managing biologics in your practice can be both complicated and risky. It can be difficult to make money – or just break even. So let’s look at three options you have for providing these often life-changing medications to your patients. Keep in mind the method you use may be dictated by the insurance company and can vary by patient. You may find that one or even all three of these options work for your practice, depending on the circumstances. It’s not necessarily an all or nothing decision!
Option 1: Specialty Pharmacy
You could order the biologic from your patient’s specialty pharmacy, and then have your patient come to your office where you administer the medication. This way, you just order the drug and manage the inventory, but the patient’s insurance (or the patient) pays for it.
Option 2: Buy and Bill
You could buy the biologic from a distributor, administer it at the office and submit claims for reimbursement to the insurance company for both the drug and administration. This process is commonly called "buy and bill".
With this option, your practice bears the cost for both the drug and administration. This can get very expensive due to the cost of the biologics. In fact, some practices take out loans to cover these expenses. As a result, you need to carefully consider the estimated costs and revenues of this scenario before proceeding. Some practices may not be willing to take on this financial risk.
Option 3: Infusion Center
With some biologics, you could send your patient to a free-standing infusion center or a hospital (if they’ll administer these meds). One possible advantage of this option is eliminating the practice’s responsibility to do the prior authorization. Some practices have been successful pushing the PA responsibility off to the infusion center or hospital, given that they would be receiving reimbursement for providing the medication. However, the practice would still need to provide patient records to the infusion center.
Weighing the Challenges
So, let’s weigh the challenges involved in these options as objectively as we can.
| Options 1 and 2 Specialty Pharmacy and Buy and Bill |
Option 2 Buy and Bill |
Option 3 Infusion Center |
|---|---|---|
|
Both are time-consuming! You must...
|
And there are more for buy and bill:
|
This is less costly, less time-consuming and you may get out of doing PAs, but...
|
(*We’ll take a detailed look at the buy and bill option, along with some tips for helping it work for you if you choose this route, in a moment.)
Keep in mind that your decision may vary by insurance carrier.
For example, patients with commercial and Medicare Advantage insurance can usually get biologics with either option 1 or 2. However, Medicare patients don’t have a specialty pharmacy option, so practices that prescribe biologics to Medicare patients must do buy and bill for those patients (option 2) or send them to a free-standing infusion center or the hospital (option 3). And some commercial payers might require you to use their own specialty pharmacy.
Most biologics manufacturers have practice resources for verifying coverage.
These services can tell you if buy and bill and/or specialty pharmacy benefits are available for your patients. Sometimes they can also tell you which method is more beneficial for the patient. You’ll get more specific information this way than you will if you simply have your practice management system check eligibility. However, use this information carefully, because sometimes it’s incorrect. Your office staff will know your specific carriers’ info much better than an outsourced benefit investigation.
The takeaway? There’s obviously no “best” or one-size-fits-all option – it all depends on your practice, your payers and your mix of patients. What we do know is that option 2, buy and bill, probably presents the most financial risk to any practice. That’s why it’s critical to estimate the profitability (revenues and expenses) – and risk – of each scenario before you make a decision.
With this in mind, let’s see how to evaluate the profitability of buy and bill.
Evaluate the Profitability of Buy and Bill
Before you begin the buy and bill option, you must figure out the costs for your practice and your expected reimbursement.
So do the analysis:
- Do your homework for each insurance company. Review your contracts to find out whether buy and bill is an option, what they reimburse, and what they require from you before they will pay.
- Research drug costs with distributors. Look into high-volume-purchasing rebates or discounts. Factor this into your analysis!
- Estimate costs for extra staff. Staff costs for all the extra work involved with biologics can be considerable. Larger practices may need a biologics coordinator (up to $60,000 a year), who ideally would have a clinical background and would be detail oriented and well organized.
- Estimate the impact on practice cashflow. Biologics are expensive, and buying them up front can be costly. How will you finance this purchase?
- Create a separate profit and loss statement for each drug so you can accurately analyze how each drug is reimbursing.
- Can you make at least a 15% profit? Or is your practice willing to accept a lower return on investment (ROI)? (A lower ROI might be acceptable for a less labor intensive payer that doesn’t require prior authorizations.)
Would buy and bill work for you? Remember, it doesn’t have to be your only option – you can use it in combination with the other two, with certain drugs and with certain insurers. You just need to make sure that the profitability of this approach will outweigh the risks for your practice.
Also, keep in mind that some insurance companies may not reimburse for biologics in a timely manner. Be sure to track profitability by insurance company – buy and bill may not make sense for some.
Tips for Successfully Navigating Buy and Bill
If the buy-and-bill option seems like a good fit for your practice, here are some tips you’ll want to follow up on to make this option as successful as possible for you.
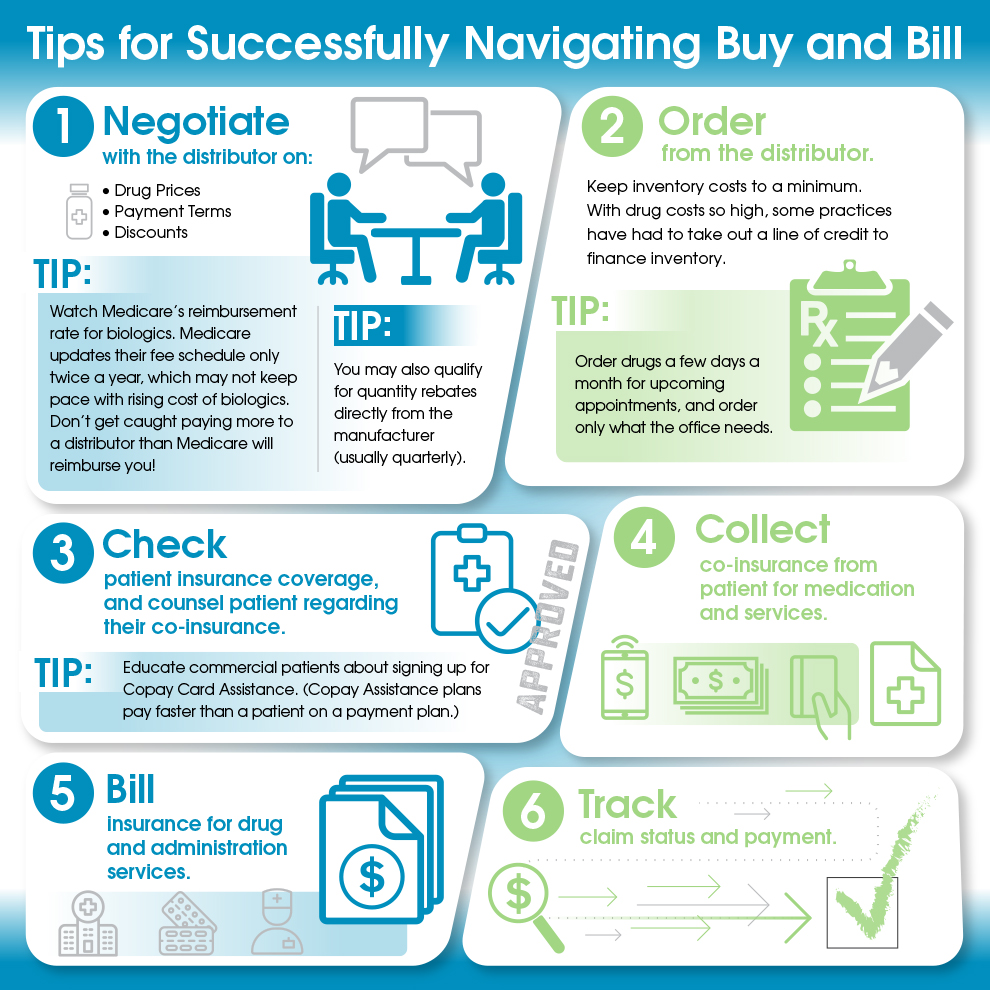
And one final piece of advice for implementing these strategies: Start with one payer and go slow. Make sure tracking and workflow are functioning well before expanding your efforts.
Reimbursement and Coding Considerations with Buy and Bill
If your practice decides to try buy and bill, you’ll want to review how Medicare and private payer insurers reimburse for medications. Here’s a handy table that lets you see the differences in reimbursement rates between Medicare and private payers:
| Medicare | Private Payer |
|---|---|
|
|
(AMGEN Assist, “Reimbursement for Physician-Purchased and Physician-Administered Drugs: Understanding the Buy and Bill Process” PDF, page 5.)
As you can see, Medicare’s reimbursement schedule is quite consistent, but when it comes to private payers, the reimbursement rates vary from insurer to insurer.
Coding for Administering Medication
How you code biologics can also make a huge difference. Here are a couple of reminders so you can get the maximum reimbursement due your practice.
Most of the time you use one of two codes for medication administration:
-
CPT 96372
Therapeutic, prophylactic, or diagnostic injection (specify substance or drug); subcutaneous or intramuscular. This code, however, reimburses very minimally! -
CPT 96401
Injection and intravenous infusion – chemotherapy and other highly complex drug or highly complex biologic agent administration. This code has a higher reimbursement, but not all insurance plans allow it; many plans require 96372 instead. If you do use 96401, make sure your documentation supports the high level of complexity needed for this code.
Check with each insurer to see if they accept code 96401. Most carriers, including Medicare, require the use of CPT 96372 but may allow multiple units of the code. And some insurance carriers will accept the billing of CPT 96401 but will only allow one unit to be billed.
Coding for Medications
When it comes to coding for physician-administered drugs, here are the codes to use:
- J0517 Fasenra
- J2182 Nucala
- J2356 Tezspire
- J2357 Xolair
- J2786 Cinqair
Newer biologics may not have assigned J-codes yet, so use a miscellaneous code, such as:
- J3490 – unclassified drugs
- J3590 – unclassified biologics
Keep in mind, though, reimbursement may take longer if you use miscellaneous codes. Plus, insurers may require you to send them invoices and additional documentation to get reimbursed.
When submitting claims, make sure the National Drug Code (NDC) and the authorization code are attached to prevent denials. You may get initial denials when submitting claims; if so, resubmitting them in a timely fashion will likely result in receiving appropriate payment.
JW and JZ modifiers for single-dose containers
Medicare requires the use of the JZ modifier for single-dose containers when there are no discarded amounts of a drug/biologic. The JW modifier is required when not all the drug/biologic in a single-dose container is used.
| Modifier | Short Descriptor | Long Descriptor |
|---|---|---|
| JW | Discard drug not administered | Drug amount discarded/not administered to any patient |
| JZ | Zero drug wasted | Zero drug amount discarded/not administered to any patient |
The JW and JZ modifier policy applies to all providers and suppliers who buy and bill biologics under Medicare Part B. The use of these modifiers is not appropriate for drugs that are from multiple-dose containers. For further details about the JW and JZ modifiers, consult the CMS’ Discarded Drugs and Biologicals JW-JZ Modifier FAQs.
Strategies for Working with Biologics
Apart from prior authorizations and the different options for providing biologics to your patients, you need to keep in mind a couple of other factors for working with biologics.

- First, make sure your biologics (and allergy extract, medications and vaccines) are insured against loss. One prolonged power outage can wipe out thousands of dollars’ worth of inventory. (Some manufacturers may cover replacements on broken or spoiled vials. Check with them to confirm – don’t assume they’ll cover!)
- Second, educate your patients. Explain to them that if the biologic is mixed in preparation for their appointment and they don’t show, then they lose that dose. They can’t get it back from the company – and worse: they’re on the hook for the cost.
Bottom line: Don’t let your practice be stuck with the cost if patients don’t keep their appointments. Some practices safeguard themselves against this by requiring patients to confirm the appointment before they mix the dose. Another option is to not mix the biologic until the patient checks in; that way you won’t have any lost doses. The only downside is the patient will have to wait during mixing.
But remember, biologics purchased by your office for Buy and Bill administration are not patient-specific drugs. You may use drugs owned by your practice for any eligible patient. - Third, educate patients regarding their financial responsibility and payment plan options. Consider having one person be the exclusive financial contact for your biologics patients. They will be an invaluable resource if there is a problem or delay with insurance payments. Given the large expense of biologics, you’re better off addressing any issues quickly so you don’t end up with a large balance.
One more resource that might be helpful for your practice is the downloadable Biologics at a Glance Cheat Sheet, which summarizes common biologics used in immunology and allergy practices. It includes their pharmacology, indications, doses, etc. It’s a great tool for both providers and staff, and you can customize it to add notes for your practice.
Conclusion
What’s the biologics situation like at your practice? Are you convinced of their value but afraid of their risks? Take some time to discuss with your practice the pluses and minuses of the different ways to provide them, and k eep these considerations in mind:
Buy and bill is not a slam dunk. If you do go the buy-and-bill route, remember that the practice will take on certain financial risks:
- the cost of the biologics
- billing and collection costs
- the risk of a narrow spread between drug cost and reimbursement
- possible additional staff to manage billing, patient counseling, and biologics ordering/inventory, etc.
And the profit margins may not be substantial. Some practices are willing to invest in buy and bill as long as they make a small profit because they believe it’s an important service to provide to patients. In their mind, continuity of care and patient convenience are paramount considerations.
But not doing buy and bill has other limitations. You won’t have much opportunity to profit or simply break even on the time spent doing prior authorizations, ordering/managing inventory, administering biologics, etc.
So the "right" answer for each practice will vary depending on your risk tolerance, priorities, and patient and payer mix.
Get creative with your options. The good news, though, is you don’t have to choose one option and stick with it forever. You could find a way to combine all three options – patient’s specialty pharmacies, buy and bill, and free-standing infusion centers/hospitals – or use different options with different patients. Your practice may even qualify for volume rebates and discounts. Just remember: One size does not have to fit all!
Do a cost-benefit analysis. Whatever course you decide to take, do consider all the risks, costs and revenue of each option before anything else. Do a financial analysis of all the alternatives you come up with. And then make a decision based on full information and thorough analysis.
Biologics are the future, so it’s worth it to make a commitment to them and figure out how to make this process work so patients – and your practice – can benefit.
Resources
- ACAAI Prior Authorization Toolkit.
- Video and whitepaper series from Novartis - hear directly from buy-and-bill experts.
Downloadable Resources
Footnotes
- 1 AMA Wire, Andis Robeznieks, "Prior authorization is a major practice burden. How do you compare?."

 Facebook
Facebook X
X LinkedIn
LinkedIn Forward
Forward